As the name implies, spermicide works as a contraceptive by killing sperm. Usually used internally, it’s a compound that kills sperm cells, preventing them from fertilizing an egg. You may find spermicide on the shelves of one of the local drug stores, but you’re more likely to find it on condoms, sponges, or other types of contraception.
While putting chemicals in your body, particularly that area of your body, can cause anxiety, spermicide is actually quite safe. Learn more about spermicide so you can decide if it’s a good choice of birth control method for you.
Key Takeaways
- Spermicide doesn’t prevent STDs or HIV.
- It is only effective by itself about 85% of the time.
- Spermicide works best when combined with other birth control methods.
- It can cause irritation or sores in the vagina.
- Most spermicides use the same active ingredient, nonoxynol 9.
- Regular use can increase the chances of yeast infection or UTIs.
What Is Spermicide?
A spermicide is a form of non-hormonal birth control. That means that it doesn’t work like the birth control pill or an implant, which regulates hormones to prevent ovulation. Other examples of non-hormonal birth control are things like condoms or a cervical cap.
How Do Spermicides Work?
In the United States, the active ingredient in almost all spermicides is a compound called nonoxynol-9 [1]. It has been in use for almost half a century and is considered very safe for use. Other spermicides are less common.
Other compounds have been tested to improve contraceptive technology and perhaps even create a spermicide also effective against HIV transmission. Unfortunately, most of these options aren’t widely available.
Spermicide is placed in the vagina, so it can prevent sperm from entering the uterus and fertilizing an egg. Spermicide does this by making it more difficult for sperm to swim, leaving them stranded after it comes into contact with the sperm cells.
Types of Spermicide
Spermicide can be found in many forms, including:
- Spermicide foam.
- Spermicide film.
- Spermicide jelly.
- Contraceptive inserts or suppositories.
- Spermicide cream.
- Contraceptive sponge.
- Spermicide gel.
How Effective Is Spermicide?
By itself, spermicide will be successful at preventing pregnancy about 85% of the time [2]. Spermicide is most often used with another form of birth control to increase its effectiveness. Most commonly, it is used with regular condoms, sponges, or other barrier methods.
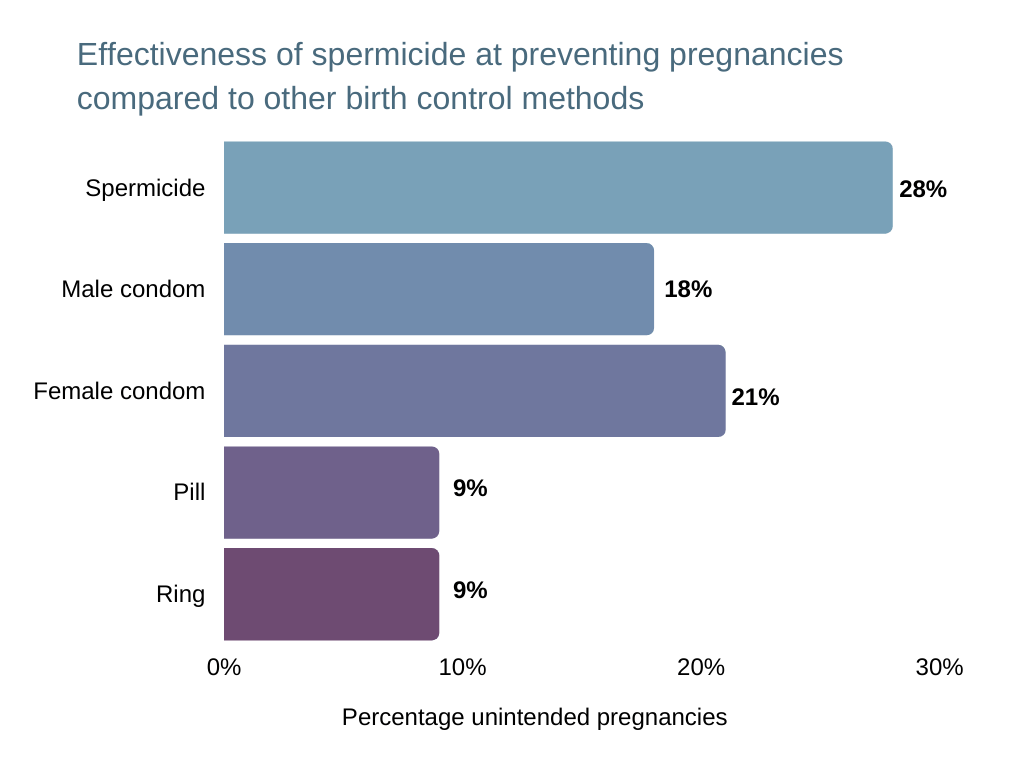
Source: https://www.cdc.gov/reproductivehealth/unintendedpregnancy/pdf/contraceptive_methods_508.pdf
In most cases, combining a barrier method with spermicide is a very effective method of contraception. That isn’t true for condoms, however. There is no evidence from peer-reviewed studies to show spermicide condoms are more effective than other condoms at preventing pregnancy.
Do Spermicides Protect Against Sexually Transmitted Diseases?
The short answer is no; spermicides do not protect against sexually transmitted diseases. The only way of contracting HIV is through fluid exchange.
While spermicide will kill sperm and prevent pregnancy, it doesn’t stop that fluid exchange. For genuine sexually transmitted infection (STI) protection, a barrier method is needed.
Regular condoms with spermicide can be used. However, spermicide condoms actually aren’t more effective [3].
How Do You Use Spermicides?
Since spermicide can come in a number of different forms, there are a few different ways you can use spermicide.
Usually, spermicide comes packaged with another effective birth control method. This is usually the case with spermicide condoms or cervical sponges. There are also a lot of different ways you can buy spermicide on its own.
Spermicide Devices
You’ll commonly find spermicide paired with a birth control sponge, cervical cap, spermicide condoms, and female condoms, for example.
Most of these devices, with the exception of male condoms, are placed inside the vagina near the cervix, where spermicide is also the most effective.
Spermicide Alone
As with a contraceptive sponge, diaphragm, or cervical cap, when you use spermicide on its own it is also placed inside the vagina near the cervix. The exact method of placing will vary depending on if it is a spermicide gel, foam, spermicide film, suppository, etc.
It is worth noting that although you’re not using spermicide with a barrier method, you can use other methods of birth control. For example, it can reduce the failure rate of natural family planning methods like the pull-out method, ovulation calculator, or fertility awareness method.
Spermicide Side Effects
While spermicide is generally considered safe, it can have some side effects to watch out for.
- Irritation: Frequent use can cause irritation or even sores to develop. The risk of contracting HIV or other STDs increases dramatically as a result [4].
- Allergic reaction: Some ingredients in spermicides can cause an allergic reaction in a sensitive area.
- Increased risk of urinary tract infections: The use of spermicide can also complicate treating UTIs.
Can Spermicide Cause UTIs?
Regular use of spermicide can increase your chances of developing a UTI considerably [5]. The odds can be as much as two or three times worse than for a woman who doesn’t use spermicide.
Basically, the spermicide makes it easier for bacteria to collect and grow within the vagina. The risk increases the more often you use spermicides.
Spermicide Advantages
Spermicide ends up in a lot of places because, despite the potential for side effects and disadvantages, it works pretty well. While it’s not truly effective on its own, there are a number of advantages to using spermicide.
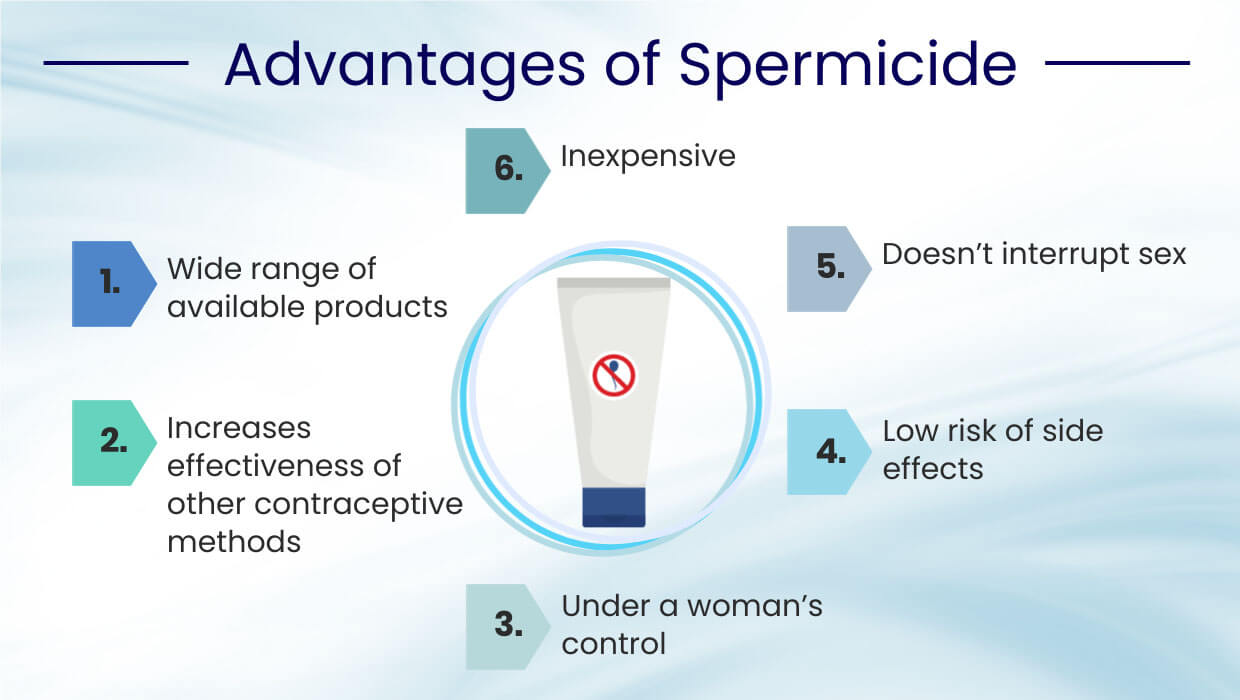
- Wide range of available products: Spermicide comes in many different forms, so you can probably find one that works for you.
- Increases effectiveness: Many methods of contraception, like a diaphragm or cervical cap, are more effective when used with spermicide.
- Inexpensive: Spermicide is one of the less expensive forms of contraception.
- Doesn’t interrupt sex: Spermicide usually has to be put in place before foreplay or sex begins.
- Low risk of side effects: While we mentioned some pretty scary side effects, those are usually pretty rare.
- Under a woman’s control: Unlike a condom, the use of a spermicide is entirely up to the woman.
What Are the Disadvantages of Spermicides?
Spermicide works well for many people, but it doesn’t fit everyone’s needs. Some disadvantages that are common when using spermicide include:
- Can cause irritation: As we’ve mentioned, spermicide can cause irritation inside the vagina.
- Increased risk of UTIs: Spermicide creates an inviting environment for bacteria.
- Inconvenient: Since spermicides need to be in place as much as 15 minutes before intercourse, you may need some foresight to protect yourself against unwanted pregnancy.
- Less effective: Spermicide isn’t really an effective method of contraception on its own.
- Doesn’t prevent STDs: In fact, in some cases, it may increase your risk.
- Uncomfortable: Spermicides have to be placed in the vagina, which can cause some discomfort.
- Shorter shelf life: Spermicide can shorten the shelf life of other contraceptive considerations, most frequently spermicidal condoms.
Doesn’t Protect Against Sexually Transmitted Diseases if Used Alone
As we’ve discussed a bit, spermicide doesn’t put up any sort of barrier. Instead, it slows down sperm and destroys the sperm cells before they can find an egg. Bacteria, viruses, and other nasties can still move between partners. As a result, spermicide won’t prevent sexually transmitted infections.
Not only is spermicide useless for preventing HIV infection, in some cases, it may also even make it more likely. Spermicide breaks down sperm cells, but it can also affect other sorts of cells as well. Irritation and even sores can appear inside the vagina, making it even easier for viruses and bacteria to enter the bloodstream.
The best option for avoiding sexually transmitted infections is condoms.
Not as Effective Against Pregnancy if Used Alone
While spermicide can be around 85% effective, that’s low compared to other methods of contraception such as condoms.
It’s most often recommended that another form of contraception be used with spermicide. Spermicide is commonly paired with a condom, despite not improving the effectiveness of condoms significantly.
Spermicide is more effective with female condoms, cervical caps, and other methods of contraception to prevent pregnancy.
FAQ
Here we answer spermicide FAQs.
Where To Buy Spermicide?
Spermicides will most likely be available wherever you can find other forms of contraception, including drug and grocery stores. If you can’t find any there and are wondering how to get birth control, you can check with hospitals or Planned Parenthood.
How Much Does Spermicide Cost?
The cost varies depending on the form and the brand. However, it’s possible to find options available for $1 an application or less.
What Brands Are Spermicides?
A few common brands include:
- Conceptrol.
- VCF.
- Trojan.
- Gynol.
- NutraBlast.
- Contragel.
Is Spermicide Safe While Breastfeeding?
Spermicide does not pass into breast milk at all, and so should be safe for breastfeeding women [6].
What Is Natural Spermicide?
Some ‘natural’ or minimally processed options have been tested for use as a spermicide. Some options tested include lemon juice, pineapple juice, and apple juice. Lemon juice was found to be the most effective.
Other compounds that have shown more promise include compounds found in plants such as saponins and tannins [7] [8].
However, it isn’t recommended to use these substances on your genitals, as they can also provoke irritation or even an infection.
How Bad Is Spermicide?
That can depend on a few different factors. Spermicide can cause irritation or even sores on the vaginal lining, leading to an increased risk of STDs. Using spermicide may also increase the chances of infection.
However, in general, it’s pretty safe. With typical use, it isn’t associated with birth defects or toxicity in breast milk [9]. It’s widely used and generally considered safe.
Conclusion
On its own, spermicide is not the best method of birth control and does have a failure rate. While it can stop and even kill sperm, it’s difficult to apply and a little too liable to fail. However, as a backup method to add a little extra security, it can be a good option.
References:
- Obstetrics, From the *Department of. “In Vitro and In Vivo: The Story of Nonoxynol 9 : JAIDS Journal of Acquired Immune Deficiency Syndromes.” LWW, 1 May 2005, journals.lww.com/jaids/Fulltext/2005/05010/In_Vitro_and_In_Vivo__The_Story_of_Nonoxynol_9.1.aspx.
- Grimes, David A, et al. “Spermicide Used Alone for Contraception.” Cochrane Library, 5 Dec. 2013, www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005218.pub4/full.
- “Sexually Transmitted Diseases Treatment Guidelines — 2002.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, www.cdc.gov/mmwr/preview/mmwrhtml/rr5106a1.htm.
- Damme, Lut Van, et al. “Effectiveness of COL-1492, a Nonoxynol-9 Vaginal Gel, on HIV-1 Transmission in Female Sex Workers: a Randomised Controlled Trial.” The Lancet, Elsevier, 1 Oct. 2002, www.sciencedirect.com/science/article/abs/pii/S0140673602110798.
- Fihn, Stephan D., et al. “Association between Use of Spermicide-Coated Condoms and Escherichia Coli Urinary Tract Infection in Young Women.” OUP Academic, Oxford University Press, 1 Sept. 1996, academic.oup.com/aje/article/144/5/512/66628.
- Serfaty, D. “Contraception Des Femmes Allaitantes : Place Des Spermicides.” Journal De Gynécologie Obstétrique Et Biologie De La Reproduction, Elsevier Masson, 23 Oct. 2014, www.sciencedirect.com/science/article/abs/pii/S0368231514001653?via%3Dihub.
- Saha, P, et al. “Evaluation of Spermicidal Activity of MI-Saponin A.” Reproductive Sciences (Thousand Oaks, Calif.), U.S. National Library of Medicine, 17 May 2010, pubmed.ncbi.nlm.nih.gov/20220105/.
- Kamboj, V.P., et al. “Semen ‘Coagulation’ – A Potential Approach to Contraception.” Contraception, Elsevier, 13 Feb. 2004, www.sciencedirect.com/science/article/abs/pii/001078247790110X.
- Gallaway, M. Shayne, et al. “The Association between Use of Spermicides or Male Condoms and Major Structural Birth Defects.” Contraception, Elsevier, 2 May 2009, www.sciencedirect.com/science/article/abs/pii/S0010782409000882.

Leave a Reply