Due to the long list of side effects of hormonal contraceptives, many women choose to use a non-hormonal option. Unfortunately, non-hormonal methods aren’t always as effective as their counterparts.
Thankfully the copper IUD is one of the most effective methods of contraception available to women, and it is entirely hormone-free.
This article investigates how it works, its side effects, pros and cons, and where and how it can be inserted should it be the best choice for you.
Key Takeaways
- The copper intrauterine device is one of the most effective non-hormonal birth control options available.
- It can be used for emergency contraception up to 5 days after unprotected sex.
- It lasts for up to 10 years.
- It does not prevent sexually transmitted diseases.
- Although it has fewer side effects than hormonal options, it may cause heavy bleeding and prolonged periods.
- The only copper IUD available in America is the Paragard IUD.
What Is the Copper IUD?
A copper intrauterine device (IUD) is a long-term, non-hormonal birth control method. It consists of a copper wire coiled around a plastic, T-shaped frame. This small T-shaped device is inserted into the uterus and effectively prevents pregnancy for up to ten years.
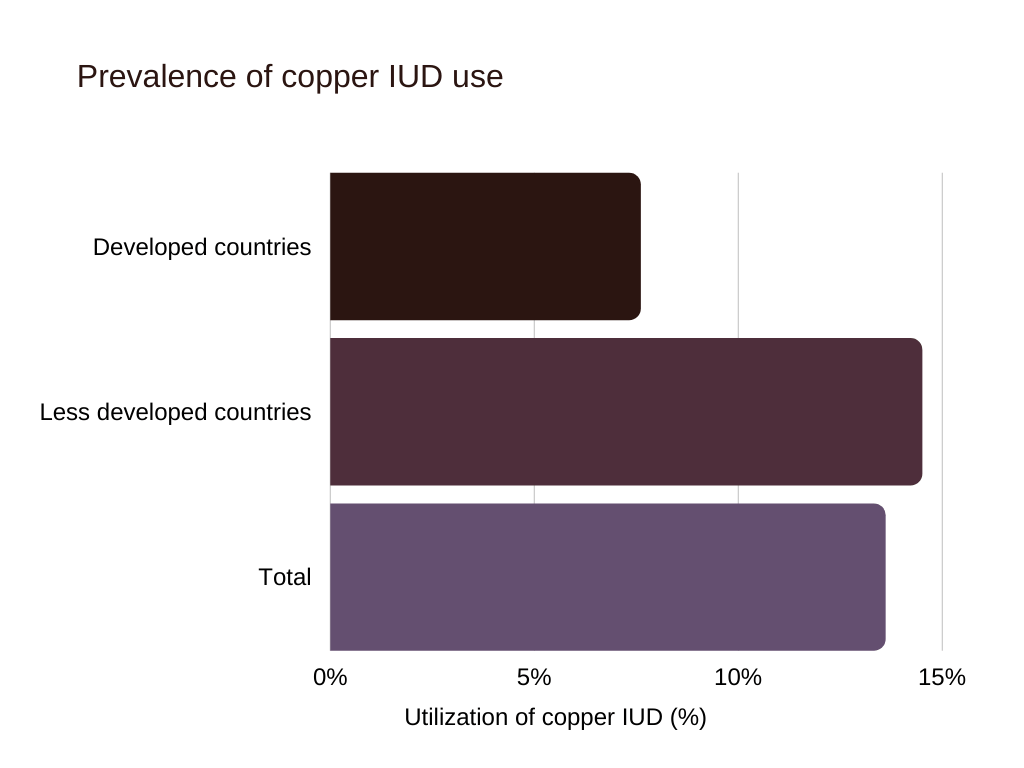
Copper IUDs are used by more than 150 million women globally and are among the most effective contraception forms available [1].
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2971735/
How Does the Copper IUD Work?
A copper IUD is inserted into your uterus through a thin tube. The copper wire coiled around the T-shaped device gradually releases copper ions into its surroundings. Unlike hormonal options, copper IUDs do not affect the thickness of the uterus lining or cervical mucus.
Instead, the copper ions released by the IUD help avoid pregnancy in two ways; by preventing implantation and by changing the direction in which sperm travel [2].
Implantation Prevention
There is some evidence that intrauterine devices, including copper IUDs, can prevent implantation of the fertilized egg from implanting in the uterine lining [3].
The copper ions released by the device cause a form of uterine inflammation that may make it more difficult for a fertilized egg to implant.
However, the copper IUD’s primary pregnancy prevention method is through:
Changing Sperm Travel Patterns
Once a woman has a copper IUD inserted, the device immediately begins releasing copper ions.
Copper ions disrupt the planned path of sperm in the following ways [4]:
- By causing localized inflammation in the uterus, the white blood cells that respond to the inflammation will kill any foreign cells, including sperm, that may enter the uterus.
- By acting on cervical mucus in a way that turns it into a makeshift spermicide. Usually, sperm must swim through the mucus to reach the uterus. However, once the copper ions act on the mucus, they either kill or make sperm unable to move.
Sperm reacts negatively to both the effect of and the copper ions themselves. This results in sperm being unable to reach the uterus or continue on their projected path toward the egg.
Sperm that can’t reach an egg can’t fertilize it.
What Is the Failure Rate of Copper IUD?
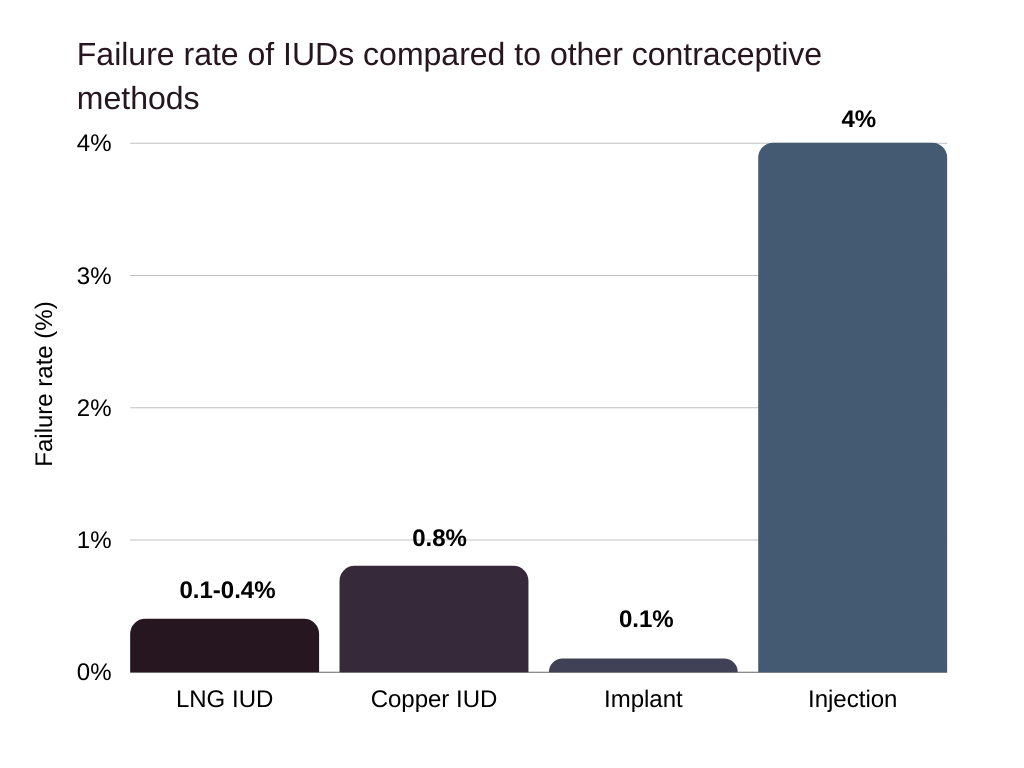
Copper IUDs are one of the most effective birth control methods available to women. With a failure rate of 0.1%, a copper IUD effectively prevents pregnancy 99.9% of the time [5].
Source: https://www.cdc.gov/reproductivehealth/contraception/index.htm
Although a copper IUD cannot directly prevent an ectopic pregnancy, which happens when an embryo implants in the fallopian tube instead of the uterus, it significantly decreases the chance of this happening compared to women using no contraception whatsoever.
The only significant threat to the overall effectiveness of copper IUDs is possible expulsion from the body.
Several risk factors may place you at an increased risk for IUD expulsion, including [6]:
- Getting an IUD inserted within four weeks of giving birth [7].
- Being under the age of 20 when the IUD is inserted.
- Having heavy or prolonged periods.
- Experiencing severe abdominal or pelvic pain during menstruation, as the muscle contractions during cramps can push the IUD out of your body.
Does Copper IUD Lose Effectiveness Over Years?
The concentration of copper ions released by a copper IUD may vary. However, the effectiveness of the device does not.
The copper IUD can prevent pregnancy for ten years, although some women have reported it maintained its effectiveness for up to 12 years after insertion [8].
Compared to the effectiveness of condoms or other forms of birth control, the copper IUD is one of the best options for women who don’t want to get pregnant and don’t want to use hormonal birth control.
Copper IUD Brands
Currently, the only copper IUDs available in America are manufactured by Paragard.
Paragard (Copper IUD)
The Paragard IUD has been FDA approved for use in the US for over 30 years since 1988 [9].
The IUD is only available via prescription and lasts for up to 10 years, although many family planning centers allow them to be used for 12 years, and they still maintain effectiveness.
What Is Copper IUD Insertion Like?
Before choosing the copper IUD as your preferred form of birth control, you must discuss it with your health care provider.
Copper IUDs are only inserted on a doctor’s prescription, and there are several contraindications for its use.
IUD Insertion Process
Before Insertion
A doctor will either conduct tests or ask for medical information to ensure you are not pregnant. They will then perform a pelvic exam to ascertain the position of your uterus.
Insertion
After a pelvic exam, a doctor will insert a tool called a speculum into your vagina to keep it open and widened.
The horizontal arms of the IUD are folded down, and the device is placed inside an applicator tube. This applicator tube is then gently inserted into your vagina, and the IUD is positioned inside the uterus.
Once the IUD is in the right location, the applicator tube is slowly pulled out, and the IUD arms are released. This may cause an uncomfortable pinch.
After Insertion
IUDs usually have one or two strings attached to them that extend into your cervix and vagina. Once the IUD is inserted, your doctor may trim these strings so that only a tiny section hangs inside your vagina.
You may experience some cramping or spotting after an IUD is inserted, although this should not cause extreme discomfort or continue for more than a few days to a week.
IUD Insertion Timing
The copper IUD can be inserted at any point during your menstrual cycle, provided you are not pregnant [10].
One of the most significant benefits of a copper IUD is that women can have the IUD inserted as an emergency contraceptive, which can help them avoid pregnancy up to five days after unprotected sex [11].
How to Prepare for Paragard Insertion
Once you and your doctor agree a Paragard IUD is the right birth control choice for you, an appointment will be scheduled for insertion.
The entire process usually takes between 15 and 20 minutes.
Although there are no specific requirements before getting an IUD inserted, some of the following steps may help make the process easier and more comfortable:
- Bring a mild painkiller like ibuprofen with you to take after the IUD is inserted.
- You can also take ibuprofen or acetaminophen an hour before your appointment to help ease some of the discomfort.
- Eat something small before your appointment to prevent dizziness.
- Stay hydrated before and after your appointment. This step is essential as your doctor will ask for a urine sample to ensure you are not pregnant before insertion.
When Does Paragard Start Working?
Unlike hormonal IUDs, Paragard prevents pregnancy from the minute it is inserted. However, due to mild cramping and discomfort, some women choose to wait a few days after insertion before having sexual intercourse, although it’s not necessary.
How Is the Copper IUD Removed?
Once the copper IUD has been in place for about ten years, or you decide to try and get pregnant, your healthcare provider can remove your copper IUD in a simple, pain-free process.
The IUD removal typically involves the use of a speculum to widen your vaginal walls. The doctor will then grasp the IUD string with a pair of forceps. Gently pulling on the strings will cause the IUD arms to fold upwards, and the entire device should easily slide out of your uterus and vagina.
If the IUD has become attached to your uterine wall, your doctor may perform a slightly more complicated procedure to remove it, called a hysteroscopy.
During a hysteroscopy, small tools are inserted into your uterus to facilitate the removal of the IUD. Sometimes anesthesia may be recommended, and the process can take anything from a few minutes to an hour to complete.
Copper IUD Side Effects
Like any other birth control method, copper IUDs have side effects that manifest with varying intensity from person to person.
The most common side effects of a copper IUD include [12]:
- Mild cramping.
- Irregular bleeding.
- Heavy or prolonged periods.
- Increased period pain.
In many cases, these symptoms will dissipate after a few months [13]. This should bring an end to any pain, heavy bleeding, or heavier periods you were experiencing.
Pelvic Inflammatory Disease (PID)
Another adverse effect of the copper IUD is the slightly increased risk of developing pelvic inflammatory disease. Although the occurrence of pelvic infection after the insertion of a copper IUD is very rare, its symptoms can be alarming. They should be made note of if you are considering using a copper IUD for birth control [14].
Symptoms of PID include [15]:
- Foul-smelling vaginal discharge.
- Lower abdominal pain.
- Pelvic pain.
- Vaginal bleeding.
If you suspect you may have PID, inform and get to your health care provider as soon as possible.
Is the Copper IUD Bad for Your Body?
Besides some uncomfortable side effects, the copper IUD should not have any adverse effects on your body and is considered safe.
Does Copper IUD Cause Weight Gain?
Since the copper IUD is not a hormonal birth control method, it does not have the same side effects as birth control pills or hormonal IUDs. The copper IUD, therefore, does not cause weight gain at all.
Copper IUD Contraindications
Before getting a copper IUD inserted, it is crucial to discuss any possible contraindications that would make you a poor candidate for the device with your health care provider.
The four main copper IUD contraindications are:
Copper Allergy
One of the most significant contraindications for a copper IUD is a possible allergic reaction to copper. The IUD releases copper ions into your uterus, which could cause symptoms like [16]:
- Hives.
- Red or inflamed skin.
- Swelling of the eyelids and labia.
Wilson’s Disease
People with Wilson’s disease experience the symptoms of copper toxicity, including weakness, itching, and vomiting [17].
These symptoms occur because this rare genetic illness makes it difficult for your liver to process and remove excess copper from your body [18]. A copper IUD releases even more copper ions into your uterus, which could worsen the disease and its symptoms.
Uterine or Cervical Cancer
Women who currently have invasive cervical or uterine cancer should not get the IUD as insertion could cause damage to the tissues of the cervix or uterus due to swelling or tumors [19].
The mild inflammatory effect of the copper IUD could also worsen the discomfort caused by the cancers.
Polycystic Ovary Syndrome (PCOS)
PCOS causes irregular bleeding, which may cause the copper IUD to move or be expelled. Usually, women with PCOS are prescribed copper IUDs on a case-by-case basis [20].
What Are the Pros and Cons of the Copper IUD?
Below are the main advantages and disadvantages of the copper IUD.
Pros
- An extremely effective form of birth control.
- It can be used for emergency contraception up to five days after unprotected sex.
- It doesn’t need daily maintenance, which is especially beneficial for younger women.
- It does not cause permanent sterilization.
- It doesn’t affect your menstrual cycle.
- Safe to use while breastfeeding [21].
- No interactions with medication [22].
- It can last for more than ten years.
- You don’t need to interrupt sex to use it.
Cons
- It does not prevent sexually transmitted infections (STIs) or HIV.
- It cannot prevent ectopic pregnancy, although the chance of having an ectopic pregnancy with a copper IUD is lower than without any contraception whatsoever.
- May cause side effects like heavy bleeding and painful periods.
- It could cause uterine perforation, although this is rare [23].
Benefits and Risks of Non-Hormonal Birth Control
Many people choose to use non-hormonal birth control methods to avoid the side effects hormonal methods cause, such as [24, 25]:
- Weight gain.
- Blood clots.
- Nausea.
- Spotting.
- Breakthrough bleeding.
- Irregular bleeding.
- Headaches.
Some of the most effective non-hormonal birth control methods include:
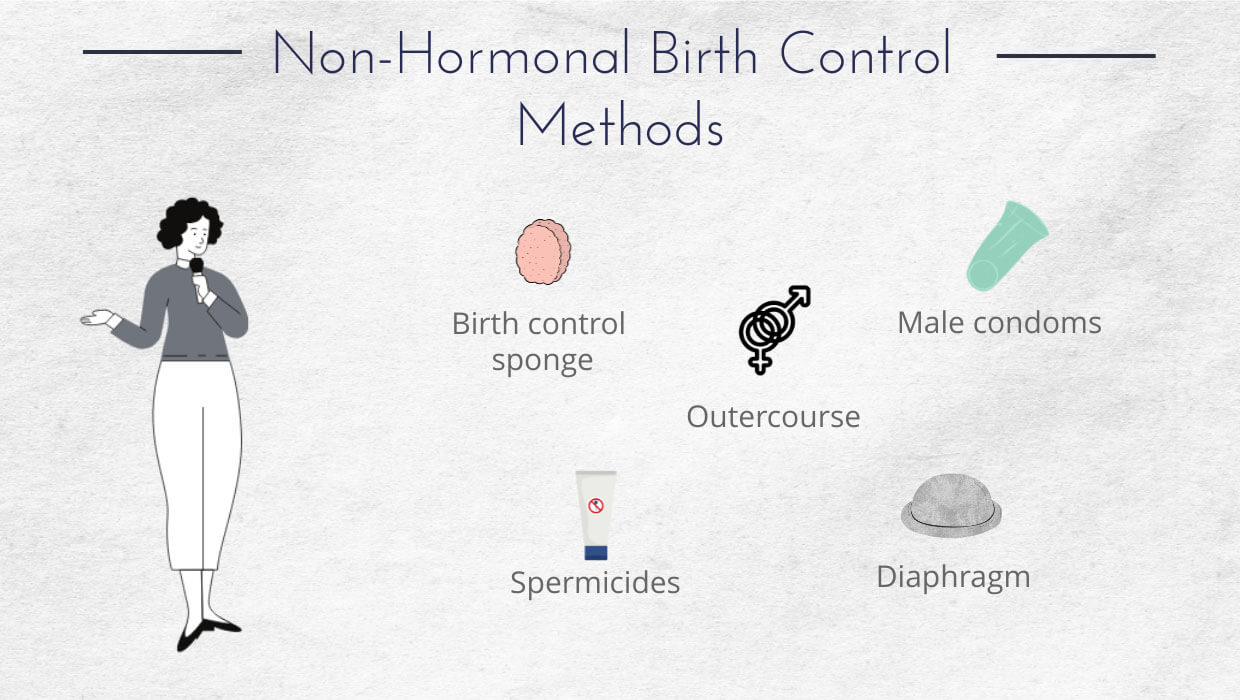
- Birth control sponge: The contraceptive sponge is a barrier that prevents possible pregnancy by releasing spermicide and blocking the path sperm use to reach the uterus. The sponge is a soft round disk that fits snugly over your cervix [26]. The birth control sponge is about 76% effective.
- Spermicides: Spermicide is inserted into the vagina before sexual intercourse. It works by preventing sperm from reaching the uterus and killing most of them in the process. Spermicides alone are about 72% effective at preventing pregnancy [27].
- Cervical cap: The cervical cap is a reusable barrier method of avoiding pregnancy. It fits tightly over the cervix and helps your body atop a possible pregnancy 94% of the time [28]. Take a look at our article on how to use a cervical cap if this seems like the right method for you.
- Outercourse: Outercourse involves having non-penetrative sex. Although there is a slight chance you can get pregnant from semen deposited outside the vaginal canal, this rarely happens.
- Male condoms: Male condoms are not only effective but can prevent the transmission of STIs and HIV [29]. It is still one of the most popular contraceptive measures available.
- Diaphragm: Similarly to the cervical cap, the diaphragm works as a barrier, preventing the passage of sperm through your cervix. It is effective around 90% of the time [30].
Despite their benefits, most forms of non-hormonal contraception are not nearly as effective as their hormonal counterparts—all except for the copper IUD that rivals even the most trusted oral or intrauterine hormonal contraception forms.
FAQ
We’ve answered some of the most frequently asked questions about the copper Paragard IUD below.
Should I Get a Non-Hormonal IUD?
Discuss using a non-hormonal intrauterine device for pregnancy prevention with your health care provider.
The best contraceptive method for you depends on various factors that cannot be answered in a blog post or article. However, if you’re in search of a form of birth control that produces minimal side effects and does not require regular maintenance, a non-hormonal IUD may be right for you.
What’s It Like to Have a Copper IUD?
Besides the unnecessary worry that your partner may feel the IUD strings, or the weird thought that a tiny device is the only thing preventing your pregnancy, a copper IUD doesn’t feel strange at all.
It doesn’t interfere with your menstrual cycle or cause severe side effects, and due to its longevity, most people eventually don’t even remember or care that it’s there until they want it removed.
Where Can I Get the Copper IUD?
The Paragard IUD is the only copper IUD available in the United States. You can have it inserted at most family planning clinics, planned parenthood centers, clinics, and hospitals.
Not only will your health care provider advise you on the suitability of a copper IUD for contraception, but they will likely also be the ones to insert the device.
If you need more information on how to get birth control, take a look at our detailed article on the subject.
How Much Does the Copper IUD Cost?
A copper IUD is likely to be covered by your insurance provider due to the affordable care act making it compulsory for all health insurance plans to cover contraceptive measures.
This means you should get a copper IUD for free or at a very low price.
Without insurance, though, copper IUDs could cost up to $1,300.
Can I Get the Copper IUD Without Insurance?
Yes, you can get a copper IUD without insurance, although this could be expensive, as they can potentially cost over $1,000.
Conclusion
If you’re looking for a non-hormonal method of contraception, the variety of choices available may be overwhelming. The copper IUD is not only one of the most effective non-hormonal birth control options available, but it lasts for over a decade.
Its relatively low maintenance, fewer side effects, and non-invasive way of working make it an excellent option for women looking to change the way they prevent pregnancy.
References:
- Kaneshiro, Bliss, and Tod Aeby. “Long-Term Safety, Efficacy, and Patient Acceptability of the Intrauterine Copper T-380A Contraceptive Device.” International Journal of Women’s Health, Dove Medical Press, 9 Aug. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2971735/.
- Kaneshiro, Bliss, and Tod Aeby. “Long-Term Safety, Efficacy, and Patient Acceptability of the Intrauterine Copper T-380A Contraceptive Device.” International Journal of Women’s Health, Dove Medical Press, 9 Aug. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2971735/.
- HB;, Ortiz ME;Croxatto. “Copper-T Intrauterine Device and Levonorgestrel Intrauterine System: Biological Bases of Their Mechanism of Action.” Contraception, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/17531610/.
- “The Embryo Project Encyclopedia.” Copper Intrauterine Device (IUD) | The Embryo Project Encyclopedia, embryo.asu.edu/pages/copper-intrauterine-device-iud.
- Goldstuck, Norman D, and Tik Shan Cheung. “The Efficacy of Intrauterine Devices for Emergency Contraception and beyond: a Systematic Review Update.” International Journal of Women’s Health, Dove, 21 Aug. 2019, www.ncbi.nlm.nih.gov/pmc/articles/PMC6709799/.
- Jatlaoui TC;Whiteman MK;Jeng G;Tepper NK;Berry-Bibee E;Jamieson DJ;Marchbanks PA;Curtis KM; “Intrauterine Device Expulsion After Postpartum Placement: A Systematic Review and Meta-Analysis.” Obstetrics and Gynecology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/30204688/.
- Jatlaoui TC;Whiteman MK;Jeng G;Tepper NK;Berry-Bibee E;Jamieson DJ;Marchbanks PA;Curtis KM; “Intrauterine Device Expulsion After Postpartum Placement: A Systematic Review and Meta-Analysis.” Obstetrics and Gynecology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/30204688/.
- Kaneshiro, Bliss, and Tod Aeby. “Long-Term Safety, Efficacy, and Patient Acceptability of the Intrauterine Copper T-380A Contraceptive Device.” International Journal of Women’s Health, Dove Medical Press, 9 Aug. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2971735/.
- Nelson, Anita L, and Natasha Massoudi. “New Developments in Intrauterine Device Use: Focus on the US.” Open Access Journal of Contraception, Dove Medical Press, 13 Sept. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5683151/.
- F;, Havránek. “[Which Stage of the Menstrual Cycle in Best Suited for the Insertion of IUD?].” Ceskoslovenska Gynekologie, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/679301/.
- TS;, Goldstuck ND;Cheung. “The Efficacy of Intrauterine Devices for Emergency Contraception and beyond: a Systematic Review Update.” International Journal of Women’s Health, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/31686919/#:~:text=Background%3A%20The%20copper%20intrauterine%20device,%2Dreversible%20contraception%20(LARC).
- Sanders JN;Adkins DE;Kaur S;Storck K;Gawron LM;Turok DK; “Bleeding, Cramping, and Satisfaction among New Copper IUD Users: A Prospective Study.” PloS One, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/30403671/.
- S;, Hubacher D;Chen PL;Park. “Side Effects from the Copper IUD: Do They Decrease over Time?” Contraception, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/19341847/.
- E;, Larsson B;Rodau S;Patek. “Pelvic Inflammatory Disease among Women Using Copper IUDs, Progestasert, Oral Contraceptive Pills or Vaginal Contraceptive Pills: a 4-Year Prospective Investigation.” Contraceptive Delivery Systems, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/12278910/.
- Jennings, Lindsey K. “Pelvic Inflammatory Disease.” StatPearls [Internet]., U.S. National Library of Medicine, 13 May 2021, www.ncbi.nlm.nih.gov/books/NBK499959/#:~:text=Women%20with%20PID%20may%20present,abdominal%20pain%20and%20pelvic%20discomfort.
- Purello D’Ambrosio F;Ricciardi L;Isola S;Gangemi S;Cilia M;Levanti C;Marcazzò A; “Systemic Contact Dermatitis to Copper-Containing IUD.” Allergy, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/8899120/.
- Chaudhry, Hammad S. “Wilson Disease.” StatPearls [Internet]., U.S. National Library of Medicine, 4 May 2021, www.ncbi.nlm.nih.gov/books/NBK441990/#:~:text=Wilson%20disease%20(hepatolenticular%20degeneration)%20is,personality%20change%2C%20seizures%2C%20etc.
- Liu, Jing, et al. “Epidemiology, Diagnosis, and Treatment of Wilson’s Disease.” Intractable & Rare Diseases Research, International Research and Cooperation Association for Bio & Socio-Sciences Advancement, Nov. 2017, www.ncbi.nlm.nih.gov/pmc/articles/PMC5735277/.
- AL;, Nelson. “Contraindications to IUD and IUS Use.” Contraception, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/17531621/.
- Felix, Ashley S, et al. “Intrauterine Devices and Endometrial Cancer Risk: a Pooled Analysis of the Epidemiology of Endometrial Cancer Consortium.” International Journal of Cancer, U.S. National Library of Medicine, 1 Mar. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4267918/.
- Rodrigues da Cunha AC;Dorea JG;Cantuaria AA; “Intrauterine Device and Maternal Copper Metabolism during Lactation.” Contraception, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/11257247/.
- Kaneshiro, Bliss, and Tod Aeby. “Long-Term Safety, Efficacy, and Patient Acceptability of the Intrauterine Copper T-380A Contraceptive Device.” International Journal of Women’s Health, Dove Medical Press, 9 Aug. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2971735/.
- J;, Heinonen PK;Merikari M;Paavonen. “Uterine Perforation by Copper Intrauterine Device.” European Journal of Obstetrics, Gynecology, and Reproductive Biology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/6378687/.
- K;, Dawson. “Side Effects of Oral Contraceptives.” The Nurse Practitioner, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/503375/#:~:text=Some%20of%20the%20side%20effects,cancer%3B%20and%2C%20hepatic%20effects.
- Kailasam, Chandra, and David Cahill. “Review of the Safety, Efficacy and Patient Acceptability of the Levonorgestrel-Releasing Intrauterine System.” Patient Preference and Adherence, Dove Medical Press, 2 Feb. 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC2770406/.
- DA;, Edelman. “The Vaginal Contraceptive Sponge.” IPPF Medical Bulletin, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/12266284/.
- R;, Raymond E;Dominik. “Contraceptive Effectiveness of Two Spermicides: a Randomized Trial.” Obstetrics and Gynecology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/10362151/.
- RM;, Secor. “The Cervical Cap.” NAACOG’s Clinical Issues in Perinatal and Women’s Health Nursing, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/1596432/.
- Marfatia, Y S, et al. “Condoms: Past, Present, and Future.” Indian Journal of Sexually Transmitted Diseases and AIDS, Medknow Publications & Media Pvt Ltd, 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4660551/.
- Schwartz JL;Weiner DH;Lai JJ;Frezieres RG;Creinin MD;Archer DF;Bradley L;Barnhart KT;Poindexter A;Kilbourne-Brook M;Callahan MM;Mauck CK; “Contraceptive Efficacy, Safety, Fit, and Acceptability of a Single-Size Diaphragm Developed with End-User Input.” Obstetrics and Gynecology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/25751199/.

Leave a Reply