A vasectomy is an effective solution to contraception methods, however, it doesn’t have to be permanent. Many men decide to have a vasectomy reversal for various reasons, but will your fertility go back to normal?
We’re looking closer at vasectomy procedures, reversals, potential side effects, and what else to expect.
Key Takeaways
- Vasectomy side effects are usually mild or rare.
- If you decide to have another child, a vasectomy reversal procedure is possible.
- Reversal surgeries are generally safe with a return to normal activity over several weeks.
- Reversals are longer, more in-depth procedures that usually require general anesthetic.
- If the procedure is unsuccessful, IVF, adoption or a donor are possibilities.
What are Vasectomy Side Effects?
A vasectomy involves cutting, separating, and cauterizing the ends of the vas deferens, which carries sperm through the penis [1]. Like all medical procedures, vasectomies do have risks, but most of these are mild.
Short Term Side Effects
Most men won’t experience side effects apart from the usual post-surgical pain, as long as they are practicing safe wound care [2]. Bleeding or hematoma is the most common side effect, affecting 4-20% of men. Primary surgical failure, where the surgery just doesn’t work, affects up to 5% of men, while infections are seen in 0.2-1.5% of cases.
After the procedure, expect some pain and discomfort, but this can usually be solved with ibuprofen. Bruising and swelling are typical too, and applying an ice pack (covered with cloth!) for 10-15 minutes at a time brings relief to all three of these after-effects [3].
The no-scalpel vasectomy is a faster, safer method if you are concerned about any of the above. The risk of post-surgical hematoma or infections is around 80% lower, for example. There is a one-third lower risk of scrotal pain and a 25% lower chance of pain during surgery. However, no-scalpel vasectomy is equally effective [2].
To ensure that any failure is picked up that may get your female partner pregnant, you should still use contraception until success is confirmed.
Long Term Side Effects
Long-term side effects include chronic pain, which is seen in 1-14% of cases. Fortunately, research shows that vasectomy is not associated with a higher risk of prostate cancer.
Vasectomy also does not leave you unable to produce sperm or cause testicular cancer, high blood pressure, or other vascular diseases [2].
Other potential long-term effects include:
- Epididymitis, inflammation of the coiled tube where sperm matures which also carries sperm to the vas deferens. Like other inflammatory issues, this causes painful swelling. It only affects 1-3% of men [3].
- Sperm granulomas are quite common, but you are unlikely to notice them. These are clumps of built-up sperm. They are generally very small, and the need for surgical removal isn’t common [3].
- Vasovenous fistula, a very rare complication where the blood vessels in the vas deferens are abnormally connected to the area. This happens when they are damaged and blood pools around them and into surrounding tissues. Symptoms include blood in semen and urine, and we recommend you call a doctor immediately if you see this, regardless of what the cause may be [4].
- Delayed vasectomy failure, which is rare and occurs in less than 1% of men. The average pregnancy risk after vasectomy is only 0.1%, one in 1,000 couples [2].
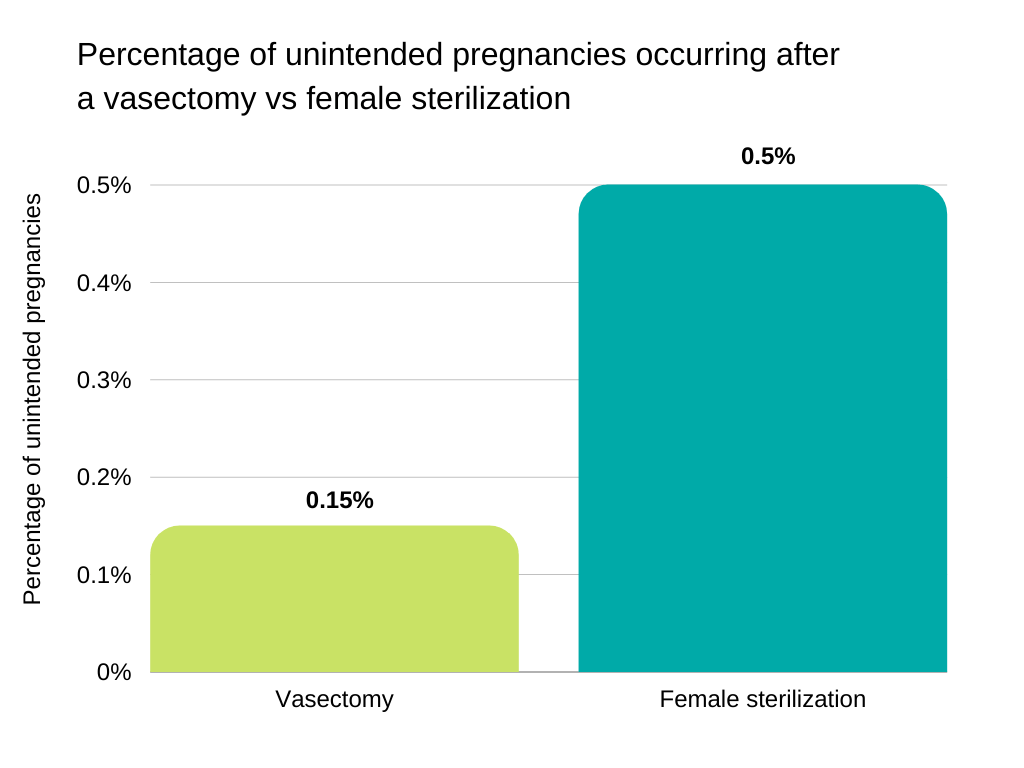
Source: https://www.cdc.gov/reproductivehealth/unintendedpregnancy/pdf/contraceptive_methods_508.pdf
Vasectomy Reversal: How Is It Done?
If you eventually change your mind and decide you’d like more children, there are some ways to reverse a vasectomy. Which one you get depends on whether or not there is sperm in your vas deferens [1]. Sometimes, the presence of enough vasal fluid indicates a simpler procedure [5].
Around 6% of men are expected to someday request a reversal, out of 175-340,000 procedures done in the USA every year [5]. They are therefore quite common, so you can easily find an experienced surgeon.
Vasovasostomy
Vasovasostomy is the medical term for a conventional vasectomy reversal surgery. Although it is an outpatient procedure, this is more complex than your original vasectomy.
Instead of being a 15-minute procedure with a local anesthetic, it takes three to four hours and usually involves general anesthesia. A vasectomy reversal reconnects the ends of the vas microsurgically [1].
During a vasovasostomy, the blocked portion of the vas deferens is removed, as it has been rendered useless and irreparable. The remaining ends of the vas deferens, which can still be functional, are then stitched together [6]. No surgical wound larger than what you would have had for a vasectomy is made.
Vasoepididymostomy
The vasoepididymostomy is more complex. If there is no viable sperm present, or there is not enough vasal fluid, your surgeon will have to connect the vas deferens directly to the epididymis [1] [5].
During a vasoepididymostomy, the surgical incision is made larger and the testicle is taken out so your surgeon can see the epididymis clearly. Then, the epididymis is cut, and the vas deferens is anchored to this new opening with initial stitches. Your surgeon finds an epididymal tubule to open up, which will be tested to find normal sperm [7].
When the presence of sperm is confirmed, the vas deferens is attached to this tubule. Your end result will not be the same as normal, but this allows for the passage of sperm once more [7].
Can a Vasectomy Be Reversed Without Surgery?
As a vasectomy involves the cutting of your vas deferens, there are no non-surgical procedures that can reverse it. They must be surgically reattached, or you will require sperm extraction and assisted reproductive intervention.
Vasectomy Reversal Recovery
Similar to vasectomies, you can usually control post-operative pain with oral analgesic drugs. You should avoid sexual intercourse for at least four weeks, and only do light physical activity for three to four weeks after surgery. Your time off work depends on how physically demanding your job is. Generally, you will also need to wear a scrotal support for six weeks [8].
Once you start having sex again, consider non hormonal birth control or male birth control until you are ready to conceive.
Can Ejaculating Too Soon After Vasectomy Reversal Damage It?
Most men need to avoid sexual intercourse for at least four weeks after vasectomy reversal [8]. This allows the wound to heal and the reconnected vas deferens to join together on their own. You don’t want to risk the stitches becoming undone, just as you wouldn’t overdo it on any other part of your body after surgery.
Alternatives to Vasectomy Reversal
The thought of surgery can be daunting—from the procedure itself, the risk of general anesthetic (if you cannot get a regional or local alternative), cost and recovery time, it’s understandable.
It is possible to conceive again without surgery, but so far, not naturally. The use of artificial insemination or IVF after sperm extraction, fortunately, carries the same success rate as reversal surgeries [9].
Sperm Extraction and IVF
Whether you don’t want surgery or you are concerned about your vasectomy reversal failing, sperm retrieval is an option. This can be by either fine-needle aspiration or extraction from either the testicles or epididymis.
It makes sense for sperm retrieval to be done during a reversal surgery, as you may be less likely to conceive naturally than you thought. A study of 163 couples found that around half of the 99 who tried vasectomy reversals first later used IVF with insemination [9].
One method of conceiving after vasectomy or a failed reversal is in vitro fertilization (IVF) along with intracytoplasmic sperm injection. ICSI can use immature sperm, and so bypasses some causes of male infertility. It involves injecting a single sperm into the egg directly [10].
ICSI is unlike traditional IVF, where thousands of sperm are placed into a dish with the egg so the “winner” can make its way in naturally. You could also need ICSI if you don’t have enough healthy sperm to get your partner pregnant or have a low sperm count [10].
Between 50% and 80% of eggs are fertilized by ICSI, but there is always a risk that it won’t develop into an embryo, or the embryo will fail to grow further [10].
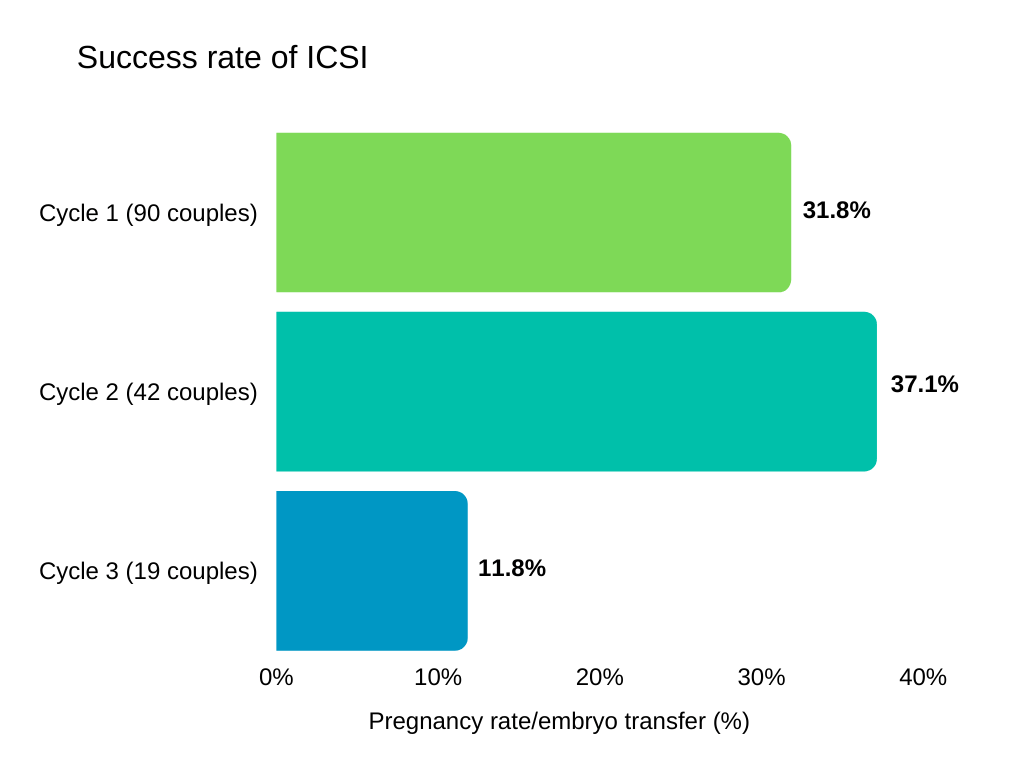
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7360402/
How Much Does It Cost to Extract Sperm After a Vasectomy?
If you choose artificial insemination, CostHelper estimates a price of $300 to $500 per attempt. With an average success rate between 10 and 20%, you are likely to need up to 10 sessions [11].
The American Society for Reproductive Medicine (ASRM) estimates a price range of several thousand dollars for sperm extraction, such as over $5,000 for microTESE (testicular extraction). IVF costs an average of $12,400 per cycle [12].
Second Vasectomy Reversal Surgery
If your first attempt fails, you can have another surgery. Common causes of vasectomy reversals’ failure include an undetected blockage somewhere in the vas deferens, or scar tissue developing in response to the trauma of your other surgeries. A second chance is somewhat less likely to succeed than the first, in both sperm flow and pregnancy rates [13].
Other Methods
If vasectomy reversals and in vitro fertilization fail, such as if your sperm count is still too low, sperm donation or adoption are options.
Adoption gives a child who would likely otherwise be bounced around in the foster system, or left in an unhappy home, a second chance at a stable, loving family. However, you must choose a reputable agency with the stability to withstand financial and legal changes [14].
Other things to consider are whether you can get to know your child’s birth mother first, and options for retaining contact after the adoption is finalized. Many parents choose an open adoption where both sides make regular contact and stay in the child’s life [14].
If you opt for sperm donation with artificial insemination, you can be assured of quality. Men who donate sperm must first be screened for genetic disorders such as cystic fibrosis. However, the number of genetic disorders tested varies, so make sure you get comprehensive screening [15].
Vasectomy Reversal Success Rate
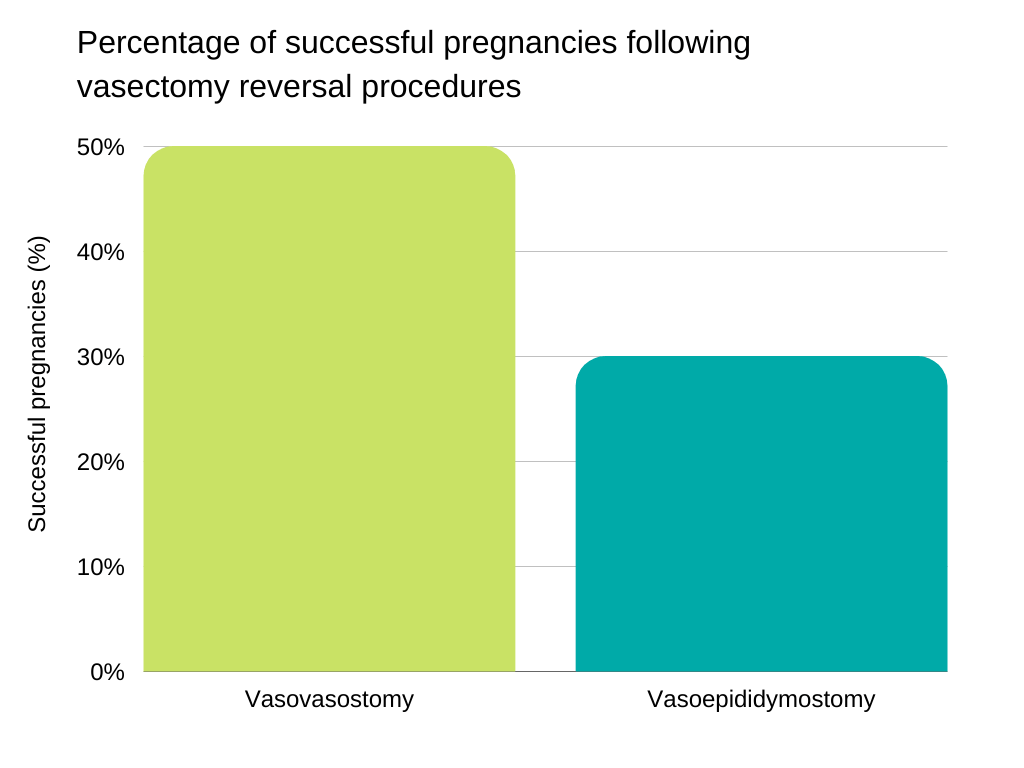
With an experienced microsurgeon, some doctors claim your chance of a successful reversal is between 80 and 90%. This figure describes your chance of sperm returning to your ejaculate. Newer robotic procedures have begun to show higher success rates with sperm returning, such as an early average estimate of 92% [8].
However, some estimates put the success rate at only 52%, measuring it by pregnancy rates within two years [6]. A 2018 review of both vasectomy reversal surgeries states that you have a 47% chance of getting your partner pregnant using current microsurgical vasectomy reversal procedures [8].
It is a myth that reversal surgeries only work on men who had vasectomies less than 10 years prior [1]. You still have a chance at success even if your procedure was 15 or 20 years ago. To avoid disappointment, doctors advise that you consider your female partner’s age and rule out any fertility problems on her side.
If you’re seeking relief from Post-Vasectomy Pain Syndrome (PVPS), you have a high chance of significant benefit. A study of 36 men with PVPS found that their average pain scores fell from 6.78 to 1.13 after surgery. As these numbers are on a 10-point scale, it shows a drop from moderately severe persistent pain to mild pain, which you may not always notice [16].
There was no real difference between vasovasostomy and vasoepididymostomy, so your chances of relief are the same regardless of what you need [16].
Vasectomy Reversal Risks
Most vasectomy reversals are without complications. One problem you may experience is scrotal hematoma, however, it is rare. One study found a rate of only seven hematomas out of 2500 procedures. No men suffered infection, and none needed another surgery to correct them. Most resolve within 12 weeks [5].
Another potential male infertility after surgery is the formation of blockages months later. Some researchers have recorded rates of 2.9-5.3%, where sperm return is only temporary. Sperm granuloma, which indicates leakage out of the tubes, is another sign of failure. For these reasons, it’s advisable to bank your sperm as soon as the flow returns [5].
Additionally, the use of general anesthetic is always risky. Compared to local anesthetic, general anesthesia has a higher risk of infection, hematoma, low blood pressure, nausea and vomiting [17].
Fortunately, you are able to choose between local or general anesthesia [5]. Easily-felt ends of the vas deferens and having your vasectomy a relatively short amount of time ago can qualify you for local anesthetic alone. Otherwise, shop around for a provider who will give you a spinal or epidural anesthesia instead.
If you are reading this because you are considering a vasectomy, consider the difference between reversal surgery and tubal ligation side effects and reversal. A tubal ligation is more invasive and women must have general anesthetic for the surgery and any future reversal.
Vasectomy Reversal Cost
The cost of a vasectomy reversal ranges from $6,000 to $15,000 in the USA, according to CostHelper. If you need the more complex vasoepididymostomy, around $700 to $1500 is added on. This includes doctor and facility fees as well as the anesthetic. Unfortunately, it is usually not covered by insurance and many plans specifically exclude the procedure [6].
Ensure that you ask the doctor what their personal success rates are with vasectomy reversals. If you wish for another child, the cost will be worth it if the procedure is successful. As some estimate that just over half of couples successfully conceive after a reversal, you must also make sure sperm banking is included [8].
Of course, you must add in time taken off work as a “cost” if you cannot get paid leave. If you are self-employed, you may have to hire a stand-in to take over certain tasks while you recover.
FAQ
In a nutshell, what are your chances of conceiving naturally after a vasectomy? We’re answering some of the most commonly asked questions.
What Percentage of Vasectomies Are Reversible?
A skilled microsurgeon gives you an 80-90% chance that your vasectomy reversal will be successful [1]. Actual pregnancy rates are unfortunately lower due to variable sperm counts, quality and fertility. Only half of couples conceive after a vasectomy reversal.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3521749/
How Easy Is It to Reverse a Vasectomy?
Although the surgery can take up to several hours, vasectomy reversal is still a day procedure and you can do light activity in a few days. Microsurgical techniques used are quite advanced so you still need to look for an experienced surgeon.
Are Vasectomy Reversals Common?
Compared to vasectomy, reversals are not as common as less than 6% of men consider them. This is, however, 6% of 175-340,000 procedures performed every year. In other words, up to 20,000 men each year are expected to wish for another child [5].
Conclusion
When looking at male birth control options, a vasectomy is a safe and permanent method. If you happen to change your mind and wish for another child, a reversal is possible, although the surgery is more complex.
If you cannot conceive, adoption or the use of a sperm donor can help you achieve your dreams of fatherhood. We wish you all the best on your journey.
References
- “Vasectomy Reversal (Vasovasostomy).” Yale Medicine, Yale Medicine, 25 Nov. 2019, www.yalemedicine.org/conditions/vasectomy-reversal-vasovasostomy.
- Zini, Armand, et al. “CUA Guideline: Vasectomy.” Canadian Urological Association Journal = Journal De L’Association Des Urologues Du Canada, Canadian Medical Association, Aug. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5110415/.
- “Long-Term Risks of Vasectomy: GLOWM.” Global Library of Womens Medicine, www.glowm.com/section-view/item/408#.YN3Yr7vivIU.
- J;, Rajan RR;Cuesta KH;Squadrito. “Vasovenous Fistula after Vasectomy.” The Journal of Urology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/9366361/.
- Herrel, Lindsey, and Wayland Hsiao. “Microsurgical Vasovasostomy.” Asian Journal of Andrology, Nature Publishing Group, Jan. 2013, www.ncbi.nlm.nih.gov/pmc/articles/PMC3739128/.
- “How Much Does a Vasectomy Reversal Cost?” CostHelper, health.costhelper.com/vasectomy-reversal.html
- authors, All, and Aaron M. Bernie. “Vasectomy Reversal in Humans.” Taylor & Francis, www.tandfonline.com/doi/full/10.4161/spmg.22591.
- Namekawa, Takeshi et al. “Vasovasostomy and vasoepididymostomy: Review of the procedures, outcomes, and predictors of patency and pregnancy over the last decade.” Reproductive medicine and biology vol. 17,4 343-355. 22 May. 2018, doi:10.1002/rmb2.12207
- Valerie, U, et al. “Pregnancy after Vasectomy: Surgical Reversal or Assisted Reproduction?” OUP Academic, Oxford University Press, 17 May 2018, academic.oup.com/humrep/article/33/7/1218/4996984?login=true.
- “What Is Intracytoplasmic Sperm Injection (ICSI)?” Reproductive Facts, www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/what-is-intracytoplasmic-sperm-injection-icsi/.
- “How Much Does Artificial Insemination Cost?” CostHelper, health.costhelper.com/artificial-insemination.html.
- American Society for Reproductive Medicine. “White Paper: Access to Care Summit.” September 10, 2015, atcwhitepaper.pdf (asrm.org).
- Patel, Abhishek P, and Ryan P Smith. “Vasectomy Reversal: a Clinical Update.” Asian Journal of Andrology, Medknow Publications & Media Pvt Ltd, 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4854082/.
- American Adoptions, Inc. “The Domestic Adoption Process [Complete Guide to How Adoption Works].” American Adoptions – How to Adopt a Child – The Domestic Adoption Process, www.americanadoptions.com/adopt/the_domestic_adoption_process_step_by_step.
- Kent D. W. Bream, MD. “Heritable Disease and Sperm Donation.” JAMA, JAMA Network, 17 Feb. 2010, jamanetwork.com/journals/jama/article-abstract/185381.
- Lee, Joo Yong, et al. “A Comparison of Epididymectomy with Vasectomy Reversal for the Surgical Treatment of Postvasectomy Pain Syndrome.” International Urology and Nephrology, Springer Netherlands, 21 Sept. 2013, link.springer.com/article/10.1007%2Fs11255-013-0517-9.
- Locke, Maren C., et al. “Assessing the Outcomes, Risks, and Costs of Local versus General Anesthesia: A Review with Implications for Cutaneous Surgery.” Journal of the American Academy of Dermatology, Mosby, 12 Jan. 2018, www.sciencedirect.com/science/article/abs/pii/S0190962218300938.

Leave a Reply