For many women, receiving ‘the pill’ for the first time is something like a rite of passage. However, birth control pills work by manipulating hormones and upsetting a woman’s natural rhythm. Some women aren’t comfortable with that for a whole variety of reasons.
There are many non-hormonal options when it comes to birth control. Each has its own advantages and disadvantages, so it’s usually possible to find one that meets your needs. All of them have one crucial advantage over hormonal birth control methods, as they leave your body chemistry alone as much as possible.
We’re going to look at the non-hormonal birth control options to see which are safe and which have the highest success rate.
Key Takeaways
- Behavioral methods of birth control are the least reliable.
- The most reliable birth control method is sterilization
- The most reliable, non-permanent birth control method is the copper IUD.
- The copper IUD is also effective as emergency contraception.
- Male condoms work best to prevent sexually transmitted infections.
- Male condoms work best for preventing pregnancy when paired with other birth control methods.
- All non-hormonal contraceptive methods have a risk of failure or side effects.
Non Hormonal Birth Control Options
Some hormone-free birth control methods are pretty common. Just about everyone has an embarrassing story about buying condoms, for example.
Many others aren’t as common or aren’t as popular as they once were. One reason the pill is so popular is that it’s a lot more convenient than fumbling for condoms mid-sexual encounter [1]. Frequently, the most effective method of birth control is the one you’ll use consistently and correctly.
When talking about the failure rate of birth control, health professionals may give two different figures. The first lists the failure rate of a method when it is used ideally, precisely as designed. The second gives the odds as observed in the field, where people may use a form of contraception incorrectly or inconsistently.
For men, non-hormonal methods are the only birth control methods available. Many people have tried to formulate male birth control pills without any success.
Barrier Methods
As the name implies, these methods use some type of barrier to prevent the sperm from meeting and fertilizing the egg [2]. The barrier can be either chemical or physical.
A barrier method may have to be put in shortly before sexual intercourse and removed shortly after. It’s generally not a good idea to leave a barrier method in place for an extended period.
Some barrier methods, such as a diaphragm or cervical cap, have been associated with toxic shock syndrome [3]. When barrier contraceptives are left in place for too long, an infection can develop. Toxic shock can be a complication of an infection and is very serious.
Both male and female condoms are considered barrier methods of contraception.
Male Condoms
A male condom is a tube that is closed on one end. A condom slips over an erect penis, forming a barrier between the penis and vagina, preventing sperm from entering the uterus.
Male condoms are considered the best way to prevent the transmission of STIs, as the barrier they form also works against viruses and bacteria.
When used in ideal circumstances, male condoms work 98% of the time. In real-world circumstances, 13 out of 100 women will become pregnant when using a condom on its own [4].
Adding another form of birth control, like spermicide, can reduce the odds of an unexpected pregnancy. Some male condoms come with spermicide.
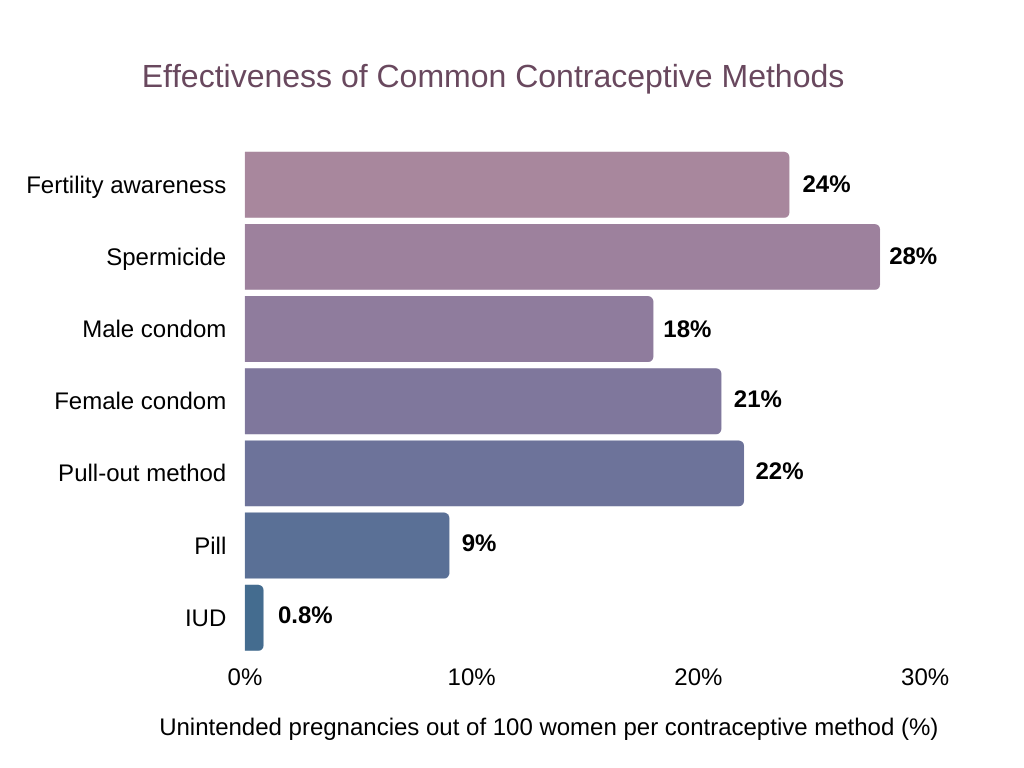 Although not the least successful contraceptive method, male condoms still failed to prevent a pregnancy in 18% of women
Although not the least successful contraceptive method, male condoms still failed to prevent a pregnancy in 18% of women
Latex is the most common material used. However, some people are allergic to a male latex condom, so condoms made from other materials are also sold.
Diaphragms and Female Condoms
Though sometimes conflated, diaphragms and female condoms are actually two different barrier methods of birth control.
A female condom can be thought of as an internal condom. They consist of a pouch, usually stiffened somewhat with rings, closed on one end. This sort of condom is inserted into the vagina with the open end remaining outside the vagina.
A diaphragm is similar. However, diaphragms are smaller and go entirely into the vagina. They are placed over the cervix to prevent sperm from traveling up into the uterus.
Both methods have to be put in place immediately before intercourse, which can be awkward. Both also have to be placed correctly in order to work well. As a result, both have a slightly higher rate of failure.
A condom for a woman will fail about 5 times out of 100 when used in ideal circumstances but will fail over 20% of the time in real-world use.
When using a diaphragm with spermicide, 6 out of 100 women in ideal circumstances will become pregnant. In the real world, 17 out of 100 will become pregnant.
Cervical cap
Cervical caps are very similar to a diaphragm. It’s a small device that fits over the cervix. A cervical cap should be used with a spermicide.
This form of birth control will fail about 9 times in 100 in ideal circumstances. In real-world use, it will fail about 14 out of 100 times.
Cervical Sponge
This method is sometimes also called a birth control sponge. It’s used similarly to a diaphragm in that it is placed over the cervix. A contraceptive sponge has spermicide on it, preventing sperm from fertilizing an egg.
As with a diaphragm, proper placement is essential. However, the advantage of the sponge is that it will continue to work for about 24 hours. You don’t need to take it out and reapply spermicide during that time.
A sponge will work about 90% of the time in ideal circumstances, though sponges are half as effective if you’ve already had children. In the real world, it works about 90% of the time.
Spermicides
While spermicides may come as creams, gels, or tablets, they are all usually some form of a compound called nonoxynol-9 [5]. It has been in use for over 30 years as a safe, effective spermicide.
As the name implies, it’s a chemical that damages sperm or otherwise prevents them from moving. In other words, spermicide kills sperm. Spermicides are frequently paired with other forms of birth control [6].
When used on its own in ideal circumstances, about 1 in 5 women will become pregnant. In the real world, a little over 1 in 4 women will end up becoming pregnant.
Behavioral Methods
Family planning may be a newer term, but it isn’t a new concept. Most methods of birth control, particularly hormonal birth control methods, were invented in the second half of the 20th century.
Natural family planning, also called natural birth control, is a term for a few different methods of non-hormonal birth control. These methods don’t depend on a barrier device like a condom. Instead, these methods work with the body’s natural rhythms or have the man attempt to avoid ejaculating inside the vagina entirely.
In general, these methods tend to have a higher failure rate.
Withdrawal (Pull Out Method)
This form of natural birth control is relatively straightforward. As a man reaches climax, he removes his penis, preventing pregnancy. The concept is clear, but the execution is sometimes tricky. This method relies largely on the self-control and experience of the man.
In ideal circumstances, only 4 out of 100 women will conceive when using the withdrawal method. In real-world cases, the odds of failure are about 20%.
Fertility Awareness Method
This method is also sometimes known as the rhythm method. It uses a variety of fertility awareness methods to track a woman’s menstrual period, allowing partners to avoid sex during fertile periods.
Fertility awareness is not an exact science. Women have to monitor their basal body temperature, which can be challenging. Some methods of detecting ovulation include testing cervical mucus, which can also be difficult. A woman’s cycle also may vary naturally. This method works best if a woman’s menstrual cycle is fairly regular.
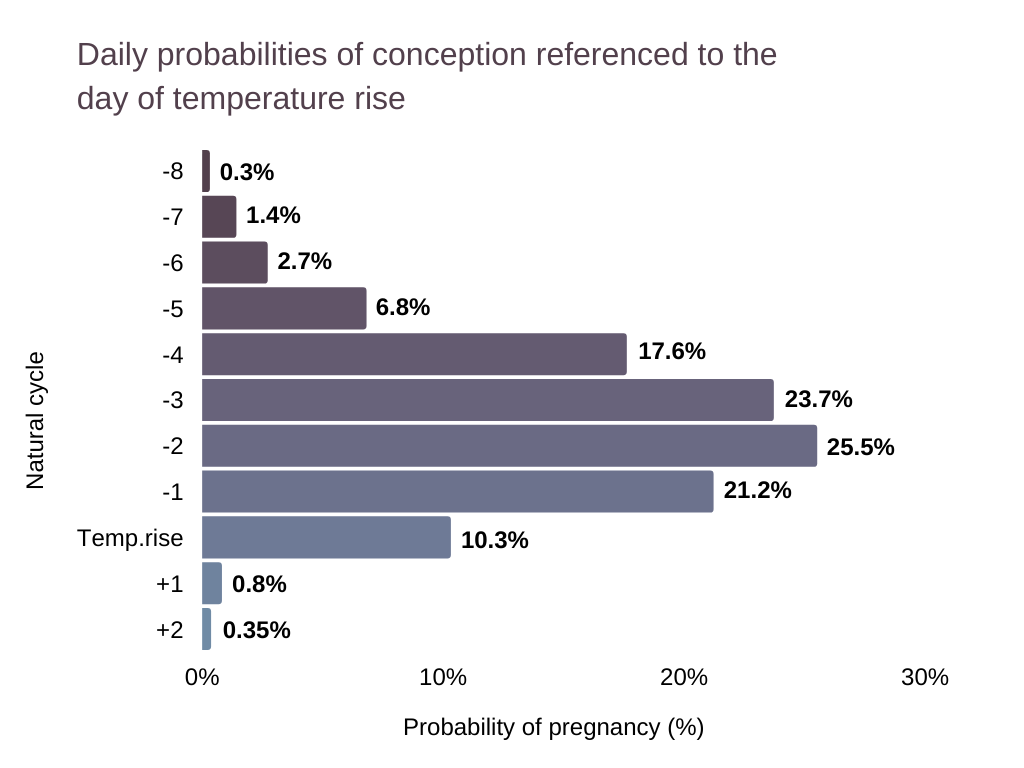 At around -5 days before temperature rise, the chances of pregnancy increase steadily before declining rapidly
At around -5 days before temperature rise, the chances of pregnancy increase steadily before declining rapidly
The success rate of this natural family planning method is about the same as other behavioral, non-hormonal birth control options. In ideal circumstances, 3 women out of 100 would become pregnant using this method to prevent pregnancy. In practice, it’s a little over 20%.
Outercourse
The name says it all. This method prevents pregnancy as, during outercourse, the penis doesn’t actually enter the vagina. In terms of birth control options, this method is preferable as even a short amount of penetration can lead to pregnancy. Additionally, there isn’t the element of self-control to consider.
In theory, this method of birth control should be 100% effective.
Copper IUD
A copper intrauterine device (IUD) is a t-shaped piece of plastic with a thin copper wire wrapped around it [7]. Strictly speaking, this method is drug and hormone-free. Instead, copper is toxic to sperm, preventing them from moving. As a result, they can’t find the egg and fertilize it.
Copper IUDs also have a second line of defense [8]. If an egg is fertilized, the copper in the IUD will make it more difficult to implant in the lining of the uterus.
It is also one of the most effective forms of emergency contraception available. If a copper IUD is inserted within 5 days of having unprotected sex, there is a 99.9% chance of preventing pregnancy. Additionally, because it’s an IUD, you don’t have to worry about misusing it.
A copper IUD can sometimes shift out of proper placement, becoming less effective. It has also been associated with increased cramping, pain, and a heavier period flow, particularly in the first few months. However, it will continue to work for over 10 years. Copper IUDs have also been linked to a higher risk of pelvic inflammatory disease [9][10].
Permanent Sterilization
Sterilization is the most extreme of the non-hormonal options for birth control. It involves a surgical procedure for both men and women. It is considered permanent.
Male Sterilization
In a vasectomy, the tubes that carry sperm are sealed [11]. While a man can still get an erection and climax, no sperm is ejaculated.
Vasectomies can be reversed. However, it requires another procedure. Both procedures come with risks of impotence or other problems. It can also affect free testosterone levels.
Female Sterilization
Female sterilization can happen in a couple of ways. With each, the egg is prevented from reaching the sperm or uterus. All of these options are permanent.
Tubal ligation may be the most common [12]. The fallopian tubes are sealed so that eggs can’t travel to the uterus.
Because the uterus and fallopian tubes have been severed, an egg that may already have been fertilized can’t implant itself in the uterine lining. Instead, it may implant itself in the lining of the fallopian tube. This condition, called an ectopic pregnancy, can’t be brought to term and poses serious risks to women’s health.
Another form is called bilateral salpingectomy, in which the ovaries are removed [13]. This is less often done as a method of contraception than to prevent cancer or treat a condition. A hysterectomy, in which a woman’s uterus is removed, is sometimes done for similar reasons [14]. These procedures can lead to low testosterone in women.
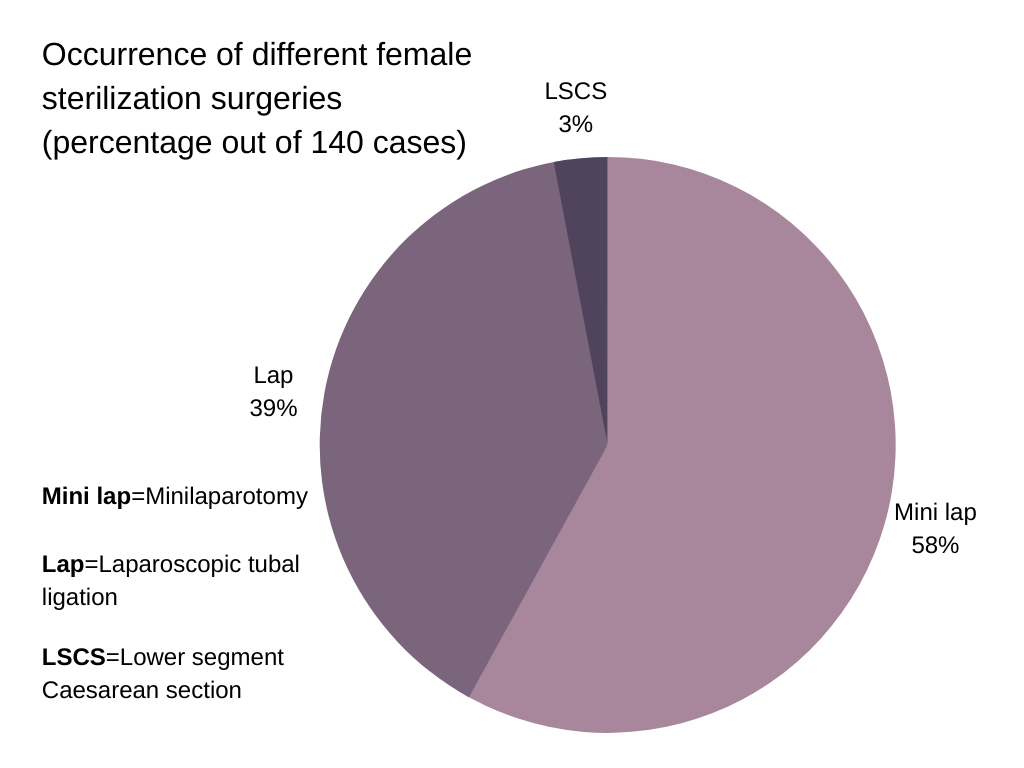 A mini lap was the most common type of female sterilization surgery performed, followed by lap. An LSCS was fairly uncommon
A mini lap was the most common type of female sterilization surgery performed, followed by lap. An LSCS was fairly uncommon
Switching to Non-Hormonal Birth Control Methods: What to Expect
Hormonal methods of birth control trick a woman’s body into not releasing an egg each cycle. When you stop taking the pill, your body’s hormones may need a little bit of time to find a new equilibrium. That may mean that a cycle may be oddly timed, be particularly strong, or be different in other ways. Preparing for those changes can be a good idea.
It can also be helpful to overlap methods of birth control. Some methods may need a bit of time to become fully effective. During that period, the chances of pregnancy may rise dramatically.
How To Choose the Right Birth Control Method for You
Certain methods of birth control are more effective statistically. However, the best form of birth control is the one that best fits your needs. As this is a decision that can potentially have life-changing consequences, it can help to think through your options ahead of time.
Factors to consider might include:
- Future plans for children.
- Other health considerations.
- Comfort and ease of use.
- Frequency of use.
- Expense.
- Reliability.
FAQ
What Is the Best Non-Hormonal Birth Control?
The most reliable form of non-hormonal birth control is sterilization. The non-permanent method with the highest success rate was the copper IUD.
What Is the Healthiest Form of Birth Control?
This can depend on several factors. Hormonal birth control pills are sometimes used to treat other conditions, for example. Copper IUDs may have the best mix of reliability and a low chance of side effects. If you have concerns, your doctor is the best person to ask.
Does Non-Hormonal Birth Control Work?
When used correctly, all of the methods we’ve outlined will work much of the time. The reliability of any form of birth control can vary.
Conclusion
While the pill has become the standard for birth control methods, it’s far from the only effective method. Many non-hormonal options are just as easy to use and reliable as hormonal birth control. Additionally, many have fewer side effects.
As with any health decision, however, statistics only go so far. Bringing a new life into the world is a big decision, and it’s usually a good idea to plan ahead. Using a reliable method of preventing pregnancy is essential and not a choice that should be made lightly.
References:
- “Estrogen and Progestin (Oral Contraceptives): MedlinePlus Drug Information.” MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/druginfo/meds/a601050.html.
- Barrier Methods of Birth Control, wa.kaiserpermanente.org/kbase/topic.jhtml?docId=hw138685.
- “Toxic Shock Syndrome.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 18 Mar. 2020, www.mayoclinic.org/diseases-conditions/toxic-shock-syndrome/symptoms-causes/syc-20355384.
- Posted under Health Guides. Updated 7 February 2020. +Related Content. “Contraception: Success and Failure Rates of Contraceptives.” Center for Young Women’s Health, 7 Feb. 2020, youngwomenshealth.org/2009/11/03/success-and-failure-rates-of-contraceptives/.
- “Nonoxynol-9.” National Center for Biotechnology Information. PubChem Compound Database, U.S. National Library of Medicine, pubchem.ncbi.nlm.nih.gov/compound/Nonoxynol-9.
- S;, Craig S;Hepburn. “The Effectiveness of Barrier Methods of Contraception with and without Spermicide.” Contraception, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/6759027/.
- Parenthood, Planned. “IUD Birth Control: Info About Mirena & Paragard IUDs.” Planned Parenthood, www.plannedparenthood.org/learn/birth-control/iud.
- “Copper IUD (ParaGard).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 11 Feb. 2020, www.mayoclinic.org/tests-procedures/paragard/about/pac-20391270.
- Kaneshiro, Bliss, and Tod Aeby. “Long-Term Safety, Efficacy, and Patient Acceptability of the Intrauterine Copper T-380A Contraceptive Device.” International Journal of Women’s Health, Dove Medical Press, 9 Aug. 2010, ncbi.nlm.nih.gov/pmc/articles/PMC2971735/.
- “Pelvic Inflammatory Disease – CDC Fact Sheet.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 19 Nov. 2020, www.cdc.gov/std/pid/stdfact-pid.htm.
- “Vasectomy.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 19 May 2021, www.mayoclinic.org/tests-procedures/vasectomy/about/pac-20384580.
- “Tubal Ligation.” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/treatment-tests-and-therapies/tubal-ligation.
- “Prophylactic Oophorectomy: Preventing Cancer by Surgically Removing Your Ovaries.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 11 Aug. 2020, www.mayoclinic.org/tests-procedures/oophorectomy/in-depth/breast-cancer/art-20047337.
- “Hysterectomy | Endometriosis | Fibroids.” MedlinePlus, U.S. National Library of Medicine, 26 May 2021, medlineplus.gov/hysterectomy.html.